Dealing with the loss of a loved one is an experience marked by intense emotions, from deep sadness to unexpected moments of joy when reliving a happy memory. Grieving is an inevitable and difficult aspect of the human experience, and there is no timeline when it comes to healing.
Understanding how to cope and deal with the loss of a loved one is an important process to overcome feelings of sadness and continue to embrace the time you had with your loved one.
[action 1]
The Grieving Process
Grief is a natural and necessary process illustrated by a wide range of emotions. Acknowledge and accept your emotions, whether you feel sadness, anger or guilt. Remember that your own grieving journey may look different than the person next to you, and that’s okay. There is no one right way to heal.
Grief can be broken down into five stages. Those consist of denial, anger, bargaining, depression and acceptance. Once you have reached full acceptance of your loved one’s death, it’s possible that the pain and sadness may never fully go away. But living with acceptance after loss allows you to cherish all the beautiful memories and shared experiences you and your loved one were able to create together.
It's important to remember that some people may move swiftly through all five stages of grief, while others may take a step back before fully moving forward. Also, every stage may not apply to you.
Ways to Cope with the Loss of a Loved One
Grieving is a difficult journey, and taking care of yourself is essential to navigate the complexities of the experience. It’s important to recognize that your emotional experience is valid and can be varied.
Express your emotions
Find healthy outlets for your grief. Many people engage in activities such as journaling, art, music or exercise. Creative expression can be a therapeutic channel for emotions that may be challenging to articulate verbally.
Maintain a healthy lifestyle
Grief can take a toll on your physical and emotional well-being. By prioritizing self-care through adequate sleep, a healthy diet and regular exercise, you’ll develop habits that contribute to strength and resilience during this challenging time.
Establish routines
During a period of grief, maintaining a sense of normalcy can be comforting. Try to stick to daily routines and responsibilities as much as possible. These familiar tasks can offer a small but reassuring sense of stability.
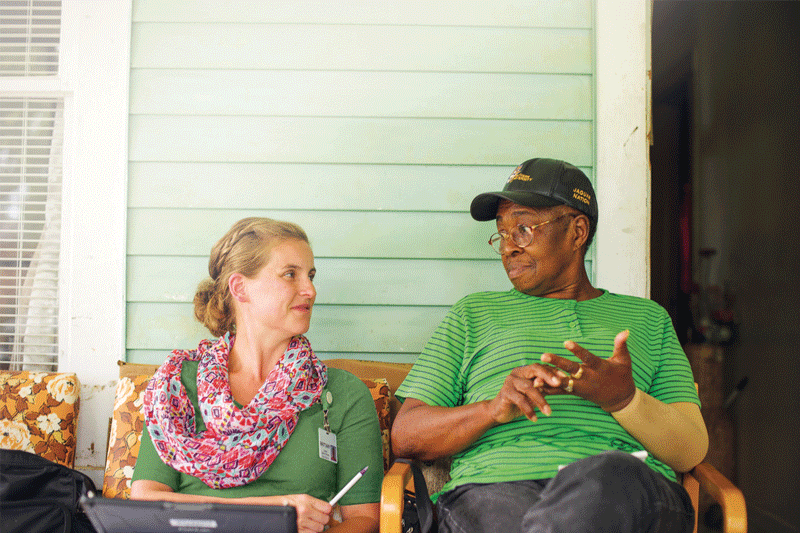
Lean on friends, family or a support group.
Grief is a shared human experience, and connecting with others who understand your pain can lighten the load of grief. Whether it’s friends, family or a support group centered around loss, surround yourself with others who can provide comfort and a listening ear.
Celebrate the life of your loved one.
Honoring the life of your loved one can be a powerful part of the grieving process. Gather with friends and family to share memories and stories to celebrate their life. Consider organizing a memorial service to ensure their memory lives on in the hearts of those who cared for them.
Seeking Professional Help for Your Grief
Although leaning on friends and family is helpful, your experience of grief may be better supported by counseling, spiritual or religious support or a support network. These resources offer tools, perspectives and guidance to find the strength to overcome emotions following loss.
Consider counseling or therapy
Grief counselors or therapists offer safe spaces to explore and understand your emotions. They provide valuable support and coping strategies to help you navigate complex emotions while offering guidance to manage your grief in the short term.
At Amedisys, our team of bereavement coordinators, chaplains and social workers are a core part of the hospice team by focusing on the unique aspect of emotional and spiritual support. Bereavement support can start as soon as your loved one enters hospice care and can continue after death.
Seek spiritual or religious support
If you are a person of faith, your spiritual or religious community can provide additional comfort and guidance during your grieving process. The rituals, traditions and support systems can provide strength and acceptance around the loss of a loved one.
Consider a support network
Online and in-person support groups connect you with a community of people who have experienced similar losses. These networks can provide comfort, support and strength, reinforcing that you are not alone in your grief.
Navigating Daily Life After a Loss
Although it might be challenging, maintaining a sense of normalcy during the grieving process is crucial. Setting realistic expectations for yourself, avoiding major life decisions and practicing patience are essential to healing.
Set realistic expectations.
Grief is a non-linear process, meaning there’s no specific timeline for how long it will last. Each person’s experience is unique, and healing happens at its own pace.
Understand that your emotions may ebb and flow and embrace the fluidity of the process. Some days will be more difficult than others, but you eventually learn how to handle your grief.
Avoid making major life decisions
Grief can cloud judgment, so it can be a challenging time to make significant life decisions. During the grieving period, try to postpone making choices that could have long-term consequences. Wait until you are in a more stable emotional state to ensure these decisions are truly what you want.
Be patient with yourself
Healing takes time, so it's important to be patient and compassionate with yourself. Accept that you will experience setbacks but remember the progress you’ve made.
Keep in mind that each step forward is a testament to your resilience.
Supporting Those Who Are Mourning
When supporting those who have lost a loved one, acknowledge that everyone grieves differently and ask if the support you hope to offer is welcomed by your loved one. Adjust your supportive efforts to whatever makes them happy.
Listen
Some people may not be ready to talk about their emotions or are too overwhelmed to understand what they mean. You can best support someone by being there for them and allowing space if they request it.
Take over specific tasks
Many people often use the phrase “let me know if I can help,” which puts pressure on your loved one grieving to communicate what they want or need. Instead, offer something more specific, such as:
- “I’d like to take you out for coffee or lunch today.”
- “I’ll pray for you and your family.”
- “I can come over tomorrow if you want company.”
- “I would be happy to help with any tasks you need help with.” This could be meal delivery, yard work or other errands.
Avoid common sayings
Common sayings can often come across as insensitive or uncaring to others. Phrases like “everything happens for a reason” or “they’re in a better place” may not align with the other person’s feelings. It’s best to not assume they have the same beliefs as you do.
Healing and growth are possible after the loss of a loved one. When you allow yourself the space to grieve, seek support, take care of yourself and find meaning in your loss, moving forward in a positive way is possible.
The bereavement team at Amedisys can help you honor your loved one and help you cope as you navigate your grieving journey. Find an online or in-person support group near you.