Attending to the spiritual needs of dying patients has been part of healthcare’s role since its earliest manifestations. Historically, in Western Europe and America, the healthcare profession was rooted in caring for the body and the soul. But this changed in the latter part of this century, as medicine identified to a greater degree with the biomedical model of healthcare.
Spirituality at the end of life is important to patients, even if they are not religious or spiritual. And patients want healthcare professionals to provide spiritual care. Meeting the spiritual needs of dying patients can improve their quality of life and outcomes, whereas lack of spiritual care has been tied to patient dissatisfaction and higher costs.
[callout 1]
The challenge of meeting the spiritual needs of dying patients has led leaders in healthcare to develop new models of practice and new codes of conduct, which specifically mention the spiritual dimension as part of good holistic care. Nowhere has the call for change become more of a reality than in the modern hospice movement, where providing spiritual care for the dying is considered essential.
How to Define Spiritual Needs
It is ingrained in human nature to connect to something bigger than ourselves. Many Americans report spirituality is important in their daily lives. Yet it is difficult to define spiritual needs because they are so personal.
[action 1]
Scholarly articles define spirituality as “the dynamic dimension of human life that relates to the way people experience, express and seek meaning, purpose and/or transcendence, and the way they connect to the moment, to self, to others, to nature, to the significant and/or the sacred.” This definition of spiritual needs captures the important fact that spirituality encompasses more than the religious. It is the part of the human being that tries to answer questions like Who am I? Why am I here? How have I lived my life? Have I made a difference?
Some questions patients often ask healthcare providers that reflect a spiritual need include:
- What will happen to me when I die?
- Why is this happening to me?
- What gives my life meaning and purpose?
- If there is a God, will He be there for me?
- How can I live now, knowing that I will die?
- How will I be remembered?
Spirituality and End-of-Life Care
Meeting the spiritual needs of dying patients and addressing spiritual pain is particularly important at the end of life. It is important that all clinicians have a basic understanding of how to treat spiritual pain. Experienced healthcare workers can often manage the physical symptoms that accompany the dying process, but spiritual pain poses unique challenges. Even the rare healthcare worker who can assess and understand spiritual pain is often at a loss to know how to help.
Spiritual Care for the Dying
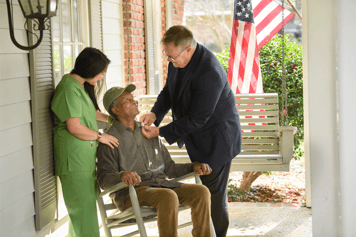
So, what is spiritual care for the dying? It can be facilitated in many ways, from helping patients find individual meaning, peace and connection to facilitating religious practices and traditions. It starts with being present for patients and making a personal connection. When the provider understands what is important to the patient – their beliefs, values and principles, and what brings them meaning and purpose – they can help facilitate spiritual healing.
Some of the things people should try to say to others to help bring closure to their loved ones are:
“Please forgive me.”
“I forgive you.”
“Thank you.”
“I love you.”
“Goodbye.”
These five little statements can have a powerful effect on patients and their families. Researchers dedicated to understanding the spiritual needs of the dying have described several important goals of spiritual care. These include hope, meaning, forgiveness, love, reconciliation, gratitude, awe, humility and surrender.
Spiritual suffering can be seen when someone is burdened by their failures or has unresolved grief or a terror of the afterlife, or simply lacks a connection with a higher power when that connection is desired. It is because of this framework of issues that Saunders insisted hospice work must be done by a team. And each team must have representatives from medicine, social work and spiritual care if they are truly to reduce the patient’s suffering.
Often, the most effective intervention for spiritual pain is acknowledging the presence of that pain and listening with empathy to the patient’s life story. This requires us to push beyond the natural tendency to try to avoid, push down or fix difficult feelings, which only creates more roadblocks to healing.
Spiritual pain is a challenging symptom. Hospice, with its philosophy of addressing all dimensions through an interdisciplinary team, is uniquely positioned to provide spiritual care for the dying. Contact an Amedisys hospice agency near you to learn more about spirituality and end-of-life care.
Reviewed by Kathleen McDonough, LCSW, MDiv, ACHP-SW, HSPC Director of Psychosocial, Spiritual & Volunteer Services